Peptide-drug conjugates (PDCs) are innovative therapeutic tools crafted to improve targeted drug delivery. By employing short chains of amino acids (peptides) connected to drug molecules, PDCs offer a strategic approach to treat diseases at their source, particularly cancer. These conjugates target specific cells, facilitating enhanced delivery precision and effectiveness. As research unfolds, the role of PDCs in therapeutic regimens may redefine how drugs interact with diseased cells, leading to breakthroughs in treatment protocols. By integrating biomedical insights with cutting-edge technology, PDCs hold promise for transforming drug delivery into a more precise science.
Understanding the Key Components of PDCs
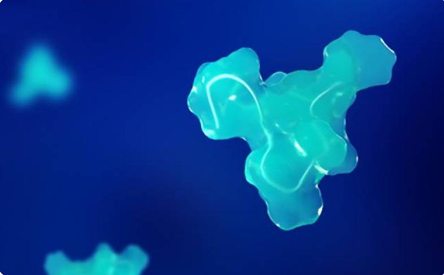
The peptide-drug conjugate consists of three fundamental components: the peptide, the linker, and the drug. The peptide acts as a homing device, guiding the payload directly to target cells by binding to specific receptors. Linkers connect the peptide and the drug, designed to release the drug at the right time and place within the body. The drug itself varies based on therapeutic needs, often chosen for its potency against specific disease targets. This unique assembly allows PDCs to leverage the selective binding capacity of peptides, ensuring that the attached drug is delivered with high specificity. In essence, each component plays a crucial role in maximizing the efficacy and safety profile of PDCs as targeted therapeutic agents.
Mechanisms of Targeted Delivery
PDCs employ sophisticated mechanisms to ensure precision in drug delivery. These include receptor-mediated endocytosis, stimulus-responsive drug release, and strategic intracellular trafficking.
Receptor-Mediated Endocytosis
In receptor-mediated endocytosis, peptides guide drugs directly to diseased cells. Peptides on PDCs recognize and bind to specific receptors on the cell surface, initiating internalization into the cell. This targeted binding triggers vesicle formation around the PDC, allowing it to enter via vesicular transport. Once inside, the PDC navigates to the appropriate cellular compartments. This precision minimizes interaction with healthy cells, drastically reducing potential side effects. Researchers design peptides with high affinity for markers overexpressed in tumors, maximizing selectivity. This method enhances drug accumulation in malignant cells, increasing therapeutic concentration at the disease site. Moreover, receptor specificity provides an opportunity to adapt PDCs for diverse therapeutic targets. With continual advancements in receptor-ligand research, receptor-mediated endocytosis remains pivotal for future PDC developments.
Stimuli-Responsive Drug Release
Stimuli-responsive drug release in PDCs ensures that the drug is freed upon sensing specific internal or external stimuli. These stimuli could be pH changes, redox conditions, or enzymes present in the targeted environment. For instance, cancer cells often exhibit a slight acidity compared to normal cells. Researchers exploit these pH differences to design linkers that break down in acidic environments, releasing the drug precisely at the tumor site. Similarly, redox-responsive linkers react to the intracellular redox potential, triggering drug liberation. This adaptability not only enhances therapeutic precision but also minimizes drug degradation before reaching target cells. The effectiveness of stimuli-responsive release systems makes them integral for delivering drugs in a controlled manner, maximizing their impact while safeguarding healthy tissues.
Intracellular Trafficking and Release
After internalization, the intracellular trafficking and release phases ensure that drugs delivered by PDCs reach their intended locations. Once inside, PDCs are transported within endosomes. Through processes like endosomal escape or enzyme-mediated cleavage, drugs are freed from endosomal compartments. This step is critical as it determines the bioavailability of the therapeutic agent within the cytoplasm or other cellular organelles. Efficient trafficking means higher concentrations of the drug reach areas like the nucleus or mitochondria, enhancing potency. By engineering peptides to navigate cellular architecture adeptly, PDCs ensure drugs reach precise intracellular targets. Advancements in understanding cellular mechanics further refine how PDCs traverse cells, optimizing drug release where it’s most needed.
Advantages Over Traditional Therapies
PDCs present distinct benefits that surpass traditional therapies, offering precision, reduced toxicity, and the potential to overcome resistance mechanisms.
Enhanced Tumor Penetration
PDCs improve tumor penetration by efficiently navigating biological barriers. Traditional treatments struggle to breach dense tumor matrices, hindering efficacy. However, PDCs, due to their peptide-based guidance systems, can target receptors overexpressed within tumors, bypassing these obstacles. Enhanced penetration ensures that drugs diffuse uniformly across the tumor, sparing adjacent healthy tissues. Innovative strategies in peptide design facilitate deeper infiltration, addressing challenges posed by heterogeneous tumor environments. As a result, PDCs deliver higher drug concentrations directly to malignant cells, substantially elevating therapeutic outcomes. This capability is pivotal in dealing with invasive and resistant cancer types, significantly improving patient prognoses while minimizing collateral damage to non-cancerous tissues.
Reduced Off-Target Toxicity
Traditional drugs often affect healthy tissues, leading to side effects. PDCs mitigate this by targeting specific cellular markers, reducing off-target interactions. By binding preferentially to diseased cells, PDCs ensure that the drug’s impact is confined to the intended site. This selectivity decreases the likelihood of systemic toxicity, allowing higher dosages without exacerbating side effects. Such a mechanism not only enhances patient compliance but also potentially broadens the therapeutic window for potent drugs. Consequently, patients experience fewer adverse reactions, fostering better treatment adherence and quality of life. With ongoing innovations in peptide specificity and linker technology, PDCs continue to refine their safety profile compared to standard therapeutic methods.
Overcoming Multidrug Resistance
Multidrug resistance remains a significant hurdle in chemotherapy. PDCs offer a novel solution by circumventing resistance mechanisms. As many resistant cells alter drug uptake pathways or express efflux pumps, PDCs target these cells directly with precise peptide guidance. By using unique transport routes or avoiding pumps altogether, PDCs ensure that effective drug concentrations reach resistant cells. Additionally, PDCs can co-deliver drugs that inhibit resistance mechanisms, enhancing their efficacy. This dual capability of targeting and overcoming resistance highlights PDCs’ potential to address recurring cases of drug-resistant cancers. By providing a focused and adaptable therapeutic approach, PDCs present a promising avenue to enhance cancer treatment resilience.
Future Perspectives
The future of PDCs in targeted drug delivery appears promising, with ongoing research poised to expand their applications. As peptide engineering advances, the specificity and binding affinity of PDCs will improve, broadening their therapeutic targets beyond oncology to include autoimmune and infectious diseases. Nanotechnology may further enhance delivery efficiency and controlled release. Moreover, the integration of artificial intelligence in designing and optimizing PDC structures could revolutionize development timelines and precision. Personalized medicine, where treatment is tailored to individual genetic profiles, might benefit significantly from PDC technology. By offering customized, targeted treatments, PDCs stand at the forefront of a new era in precision medicine. The cumulative impact of these advancements could redefine the landscape of drug delivery systems globally.
Conclusion
PDCs represent a transformative approach in targeted drug delivery, offering numerous advantages over traditional therapies. By delivering drugs with unparalleled precision, reducing toxicity, and overcoming resistance, PDCs enhance treatment efficacy and patient quality of life. As research continues to evolve, the potential of PDCs to diversify treatment paradigms becomes increasingly evident. These advancements not only promise to improve current therapeutic strategies but also pave the way for new opportunities in treating complex diseases. With ongoing innovation, PDCs could revolutionize how the medical community approaches disease management, ultimately leading to better patient outcomes and personalized healthcare solutions.

